Ready-to-Use Vials – Pharma Packaging Overview
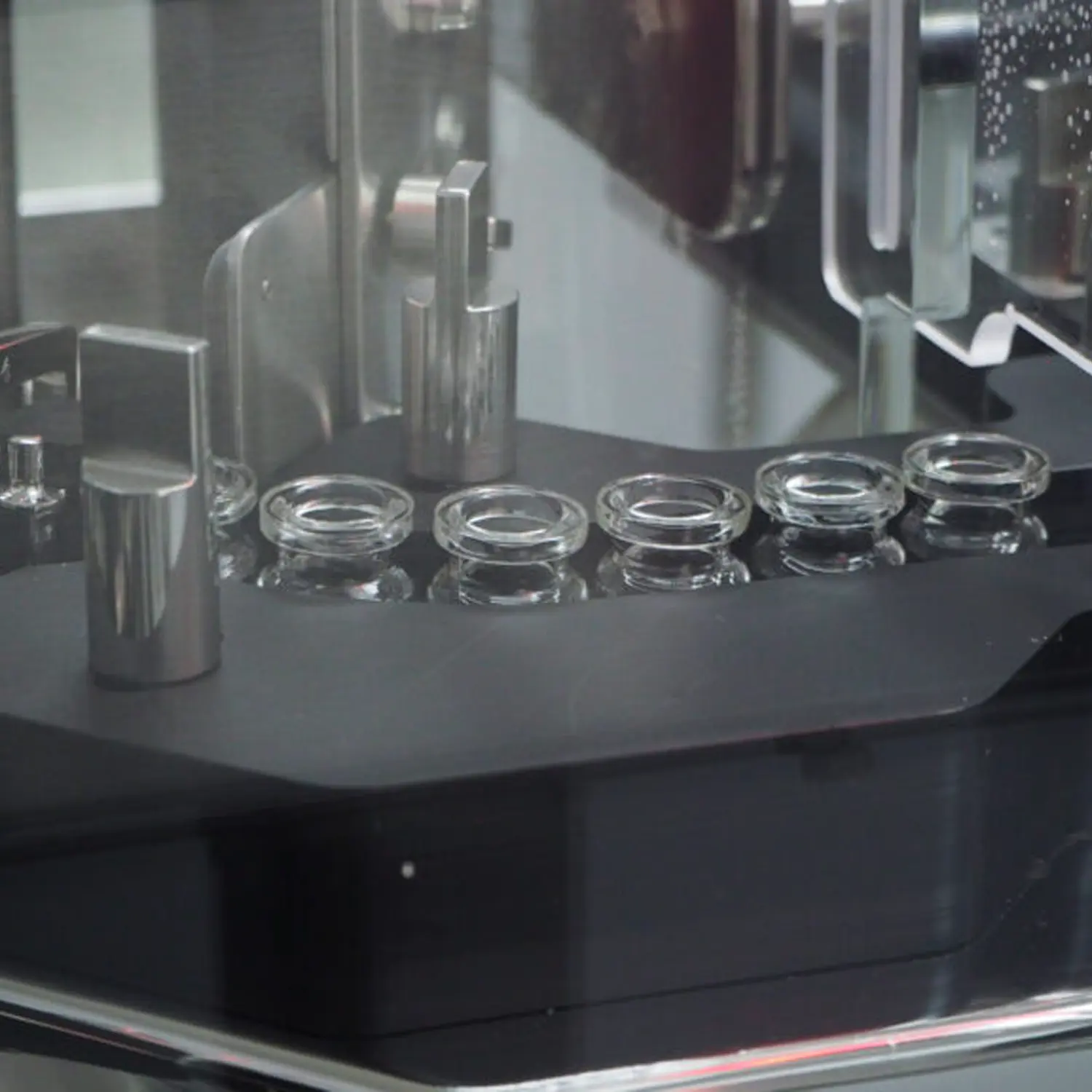
Ready-to-Use (RTU) Pharmaceutical Glass Vials
Ready-to-use vials are supplied in a form that can be immediately filled without further processing. This requires that the vials are cleaned to remove particles and chemicals, depyrogenated to remove endotoxins and terminally sterilised. The vials are often supplied with appropriate stoppers and caps to close the vial post filling. RTU glass vials are available in a wide range of sizes and specifications. If the vials are to be used for human injectables then they will comply with the requirements of the ISO 21882 standard.
Manufacture of Ready-to-Use (RTU) Glass Vials
Ready-to-use glass vials are initially produced in the same way as standard glass vials. Post manufacture, the vials are either additionally treated or sent to a new facility for further treatment.
– Washing. This process is undertaken normally with an automated washer. The washer will spray the vials internally and externally with pressurised, heated high-quality water. If the vials are to be used for human injectables then water for injection quality water is to be used. Detergents can be used if necessary but must be fully removed from the vial during the wash process. Drying of the vials is undertaken using compressed filtered air that meets at a minimum ISO 8573-1 standard 2,2,2.
– Depyrogenation. This process is undertaken using a heated oven and has an objective to remove endotoxins from the vials. A typical cycle is to heat the vials for 250°C for at least 30 minutes. This process will provide a minimum of a 3 log reduction in endotoxins. The air in the oven must be filtered to avoid recontamination of the vials with particles during the process.
– Terminal Sterilisation. This process consists of packing the vials within a sterile barrier and then sterilising the vials using either ethylene oxide or moist heat (steam). The packing process is undertaken within a cleanroom (ISO Class 5) to avoid contamination of the vials. The packaging used is designed to both protect the vials from damage or microbial contamination before filling. Sterilisation is undertaken using a cycle that will achieve a sterility assurance level of 10ˉ6. Ethylene oxide sterilized vials will have the residual ethylene oxide removed at the end of the cycle through a process known as aeration.
The final RTU packed glass vials can be stored for up to 5 years before use depending on the sterile barrier packaging used.
Testing and Certification of RTU Glass Vials
Vials for use with human injectables will be certified to show compliance with ISO 21882. This certification requires testing of the final processed vials for sub-visible particles and endotoxins. The sterilisation cycle used will be validated per ISO 11135 for ethylene oxide or ISO 17665 for moist heat. The packaging used will be validated per ISO 11607.
Additional tests on the processed vials that may be undertaken include sterility, visible particles, TOC (total organic carbon) and ethylene oxide residuals.
Benefits of RTU Glass Vials
The alternative approach to RTU vials is for the organisation to fill the vials to process them before filling. There are several disadvantages to this.
1. As there is no terminal sterilisation before filling it is critical that the vials are protected from microbial contamination after the depyrogenation process and before the filling process. Even with the best procedures, it is not possible to match the sterility assurance level of 10ˉ6 achieved with terminal sterilisation with an inline process.
2. An inline process requires significant investment in equipment and facilities. This may not be practical for organisations filling small numbers of vials.
3. The processing of vials before filling requires a series of batch tests including sub-visible particles and endotoxins. With ready to use vials these tests are completed before filling. With inline systems, a test failure can lead to a full batch being rejected.
RTU Packaging at Andersen Caledonia
Andersen Caledonia has set up the first dedicated contract site for RTU pharmaceutical packaging in Europe with the full range of services required to perform all tasks required at a single location. Contact us to find out what we can do for you here.
Article written by Jonathan Lintott, Managing Director.
Share: